Jacqueline Phang
Speech Therapist
Swallowing is a complex process involving many nerves and muscles. A swallowing disorder, or dysphagia, may result if any of these are impaired.
With a swallowing disorder, there is the danger of food, liquid or even the patient's own saliva going into the lungs rather than the stomach. This is known as aspiration. Where a patient does not trigger a cough (protective reflex) after aspirating, this is known as silent aspiration.
Aspiration may result in pneumonia, which will complicate the course of recovery. Incidence of pneumonia was found to be 4.5 times higher in stroke patients who aspirated than those who did not (Holas et al, '90). In some cases, aspiration may lead to severe breathing difficulty and/or death (Kikuchi et al, '94).
There are four phases in the swallowing process (Logemann, '83 ).
The phases of swallowing
Phase One
Our tongue, jaw and muscles of mastication manipulate the food or drink into a cohesive mass while the lips remain closed to ensure no food or drink spills out. This phase may take a longer or shorter time depending on the taste and texture of the food or drink. For example, we may chew for longer on something delicious.
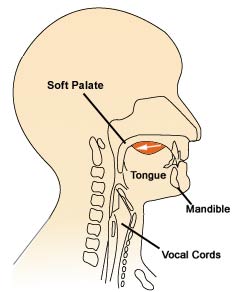
Phase 1: Manipulation into a cohesive mass
Impairment here may result in food or drink spilling. Poor secretion of saliva will result in difficulty forming the food or drink into a cohesive mass.
Phase Two
The tongue pulls the food or liquid against the roof of the mouth to the back of the throat so that a swallow may be initiated.
If there is weakness in the lips, jaw, tongue or cheeks, food and drink may spill out of the mouth, collect in the cheeks or on the tongue.
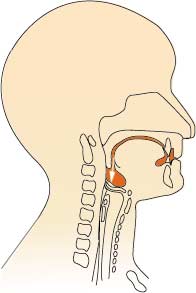
Phase 2: Pulling food or drink to back of throat
Phase Three
The swallow is triggered and the food or drink passes into the throat. At this point breathing stops momentarily and the airway is closed to prevent aspiration. This phase takes about one second.
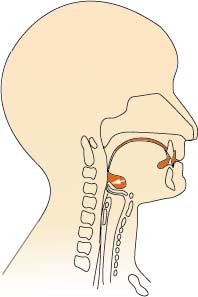
Phase 3: Swallow triggered
Problems at this phase could result in weak, delayed or absent swallows. Breathing difficulties are likely to result in aspiration.
Phase Four
The food or drink passes into the oesophagus and takes about 5-20 seconds to travel to the stomach.
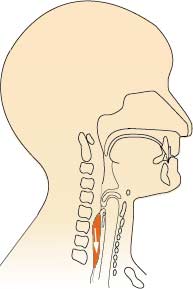
Phase 4: Food or drink passing into oesophagus
Impairment at any or a combination of the four phases may have serious implications for the patient.
Common causes of swallowing disorders
Some of the possible causes include:
- traumatic brain injury, e.g. as a result of road traffic accident
- cervical spinal cord injury
Complications may follow a swallowing disorder. More commonly, these are:
- pneumonia as a result of aspiration
Seeking help from a Speech-Language Therapist
In general, referral to a Speech-Language Therapist (SLT) in government hospitals must be made by a medical practitioner. Self-referrals are possible at private hospitals and private speech-language therapy clinics.
The following symptoms could indicate a swallowing disorder and warrant an assessment by a SLT:
- difficulty starting a swallow
- chest infection or pneumonia
- severe breathing difficulty
- coughing or choking during or after eating and drinking
- food residue in the cheek or on the tongue after swallowing
- excessive drooling especially after eating
- "gurgly" voice quality after eating or drinking (McCurtin, '97)
Assessment by a SLT
The SLT will usually begin by checking if the patient has a history of medical conditions and/or symptoms such as those described above. This may require taking a verbal history from the patient and his/her relatives.
Next will be an examination of the oral structures (i.e. lips, tongue, jaw, teeth etc) to look for asymmetry, range and strength of movement of each of these structures.
Small amounts of food, drink or ice chips may be used to assess a patient's ability to initiate and co-ordinate swallows.
Following the above, recommendations will be made regarding the patient's ability to swallow safely and modifications to diet, feeding method and the use of compensatory swallowing strategies.
The whole procedure may take between 30 minutes to 1 hour depending on the patient's ability to follow instructions and co-operation.
Multidisciplinary team approach
In cases where the patient is unable to sit up independently, positioning will be carried out by the Physiotherapist. The Physiotherapist also helps to monitor and manage the patient's chest and respiratory condition.
Recommendation for alternative feeding equipment to compensate for hand weakness or incoordination will be made by the Occupational Therapist.
A Dietitian will evaluate the nutritional needs of the patient and plan a feeding regime bearing in mind the patient's level of alertness, swallowing ability and amount of calories needed to carry out therapy
The management of a swallowing disorder often involves a team approach in hospitals. The most important members of this team are the patient and their carers. The carers could be either family members and/or nursing staff. Education is an important part of the management to ensure that carers and patient understand why s/he needs to feed in a different way.
Diagnostic procedures
When the SLT suspects that a patient may be at risk of aspiration, particularly silent aspiration, an instrumental assessment will be recommended.
Currently, there are two types of assessment available, videofluoroscopy and fibreoptic endoscopic evaluation of swallowing (FEES) (Langmore et al, '88).
A videofluoroscopy is an X-ray procedure that allows a view of the head and neck. During the procedure, food and drinks of various consistencies, mixed with a barium powder is given to the patient. It allows the SLT to observe the four phases of swallow and determine if aspiration or silent aspiration occurs. The patient is required to go to an X-ray suite. No fasting is required before this procedure.
FEES allows for a similar view except it requires the SLT inserting a small flexible fibreoptic scope (diameter of 2.5mm - 3.4mm) into the nose and down to the back of the tongue. The patient will be given food and drink of various consistencies coloured with food dye.
Differences between the two procedures include:
Decisions regarding which assessment method to use will be discussed with the patients and their family.
Treatment options
Therapy will vary depending on the cause and severity of the swallowing disorder. Therapy is broadly divided into direct and indirect, where direct therapy involves use of food and indirect does not.
Examples of direct therapy include the use of strategies such as tilting the head forward onto the chest before each swallow. The aim is to alter the dimensions of the throat and to redirect the flow of food or drink without increasing the patient's effort. Other types of therapy include modifying food and drink consistencies and to improve oral sensory awareness.
Indirect therapy involves exercises to improve the strength, speed, range and co-ordination of movements.
Factors influencing prognosis
These include:
- cause of swallowing disorder
- severity of swallowing disorder
- other medical conditions e.g. chronic lung disease, presence of gastroesophageal reflux
- patient's level of mobility
References:
- Holas, M.A., DePippo, K.L., Reding, M.J. (1994). Aspiration and Relative Risk of Medical Complications Following Stroke. Archives of Neurology, 51, p.1051-1053.
- Kikuchi, R., et al (1994). High Incidence of Silent Aspiration in Elderly Patients with Community- Acquired Pneumonia. American Journal of Respiratory Critical Care Medicine, 150, p.251-253.
- Langmore, S.E., et al (1988). Fibreoptic Endoscopic Examination of Swallowing Safety: A New Procedure. Dysphagia, 2, p.216-219.
- Logemann, J.A., (1983). Evaluation and Treatment of Swallowing Disorders. San Diego, College Hill Press, Inc.
- McCurtin, A. (1997). Clinical Indications of Aspiration Checklist. From The Manual of Paediatric Feeding Practice, United Kingdom, Winslow Press Ltd, p.15.
Date reviewed: 11 May, 2005